United HealthOne Dental Insurance
Underwritten by Golden Rule Insurance Co
United HealthOne is the largest singular healthcare provider in the country. As such, they offer great choices for dental insurance for Arizona residents
Our Rating: ★★★☆☆
Why should I consider this coverage?
Plus, you can add vision benefits
Your eyes are an important part of your health too. You can add vision benefits (available in most areas for additional premium) to your dental plan as well. Coverage for eye exams to contact lenses. Add it today for additional coverage.
Family-friendly dental plans
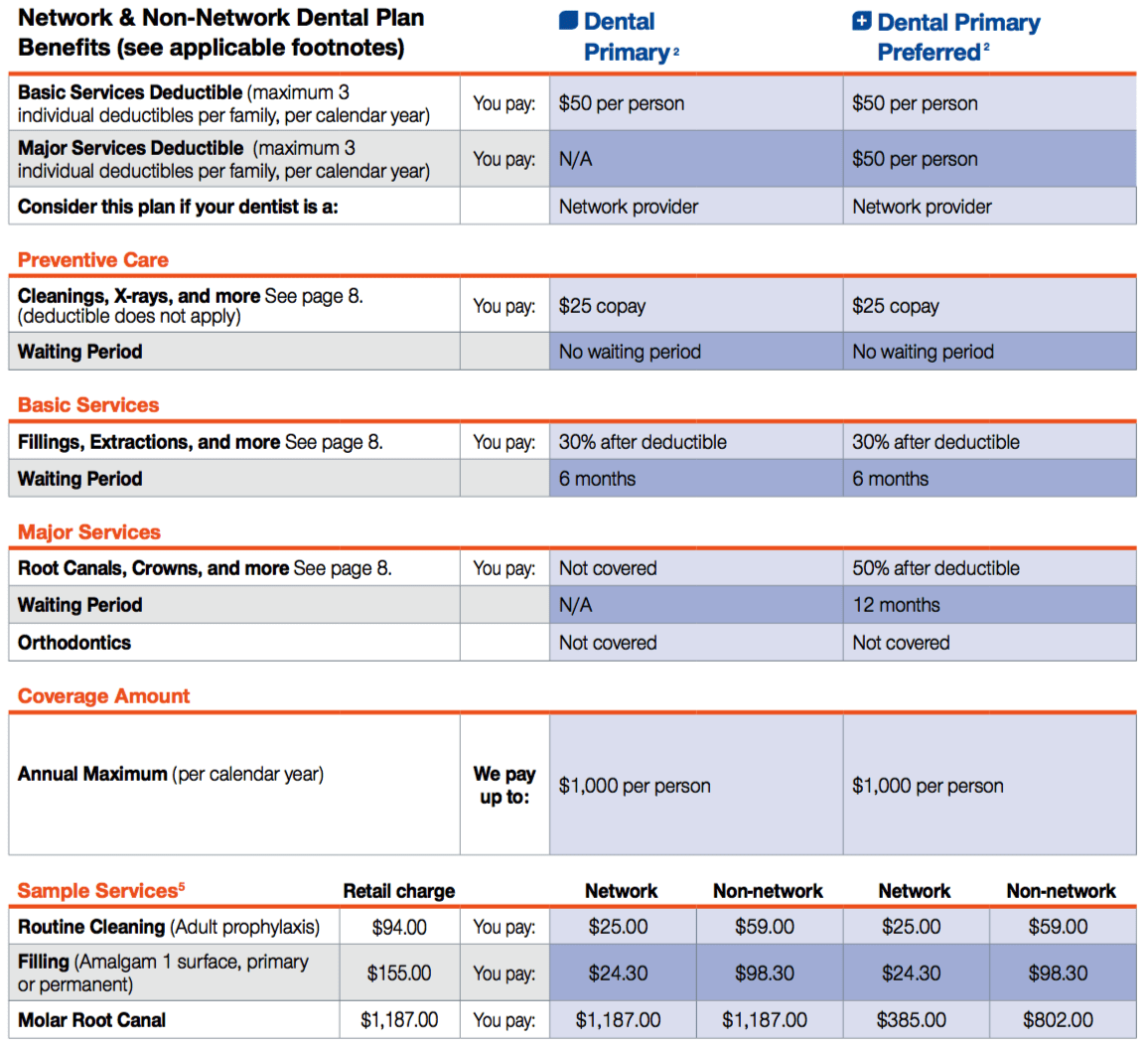
Preventive care has no waiting period and depending on the plan design, you pay a $25 copay or nothing. For Basic and Major Services, there’s a maximum of 3 individual $50 deductibles per family, per calendar year. Our Premier plans offer a combined deductible for Basic and Major services – especially helpful for large families.
Dental care at any age
No age limit means even those covered by Medicare can apply. Good dental health is important at any age. We have plans to fit your age and stage of life.
Four Dental Plans
UHC offers four plan designs. “Primary” plans have a lower maximum benefit (yearly payout cap), while “Premier” plans have a higher benefit that increases over time. From their, you can choose a plan that better suits you depending on whether or not your doctor is in network.
- Plan availability varies by state
- Pays non-network provider benefits based on the network negotiated rate. Non-network dentists can bill a patient for any remaining amount up to the billed charge. Plan availability varies
- Pays non-network provider benefits based on the reasonable and customary charge. Non-network dentists can bill a patient for any remaining amount up to the billed charge.
- If the effective date is prior to July 1, Year 2 begins the following January 1. If the effective date is on or after July 1, Year 2 will begin January 1 following 12 consecutive months of coverage. Subsequent years after Year 2 will begin the following January 1.
- Service pricing for ZIP Code 432– and assumes $50 deductible has been satisfied. Discounts vary by type of provider, geographic area, and type of service.
What's Covered
All Plans: Preventive Services Preventive services are covered without a deductible, coinsurance, or waiting periods. Dental Primary and Dental Primary Preferred have a $25 copay for preventive services.
- Oral evaluations – limited to 2 per calendar year.
- Routine cleanings – limited to 2 per calendar year.
- Fluoride treatments – limited to covered persons under the age of 16 years, limited to 2 times per calendar year.
- X-rays (bitewing) – limited to 1 series per calendar year.
- X-rays (full mouth panoramic) – limited to 1 per 36 months.
- Space maintainers – limited to covered persons under the age of 16 years, once per 60 months. Benefit includes all adjustments within 6 months of installation.
- Sealants – limited to covered persons under the age of 16 years and once per first and second permanent molar every 36 months.All Plans: Basic ServicesBasic services are covered subject to the deductible, coinsurance, or waiting periods. Basic services have a 6-month waiting period.
- Fillings (amalgam and composite).
- Simple nonsurgical extractions – limited to 1 per tooth, per lifetime.
- General anesthesia – in conjunction with oral surgery or the removal of 7 or more teeth.
- Local anesthesia.
- Palliative treatment – only if no other services other than exam and radiographs were done on the same tooth during the visit.
Provisions & What's Not Covered
Change or Misstatement of Residence (Address)
You must notify us within 60 days of changing your residence. Your premium based on your new residence will begin on the first due date after the change. If you misstate your residence on the application or fail to notify us of a change of residence, we will apply the correct premium on the first due date you resided at that residence. If the change results in: lower premium, we will refund any excess; higher premium, you will owe us.
Network providers have agreed to discounted pricing for covered expenses with no additional billing to you other than the copayment, coinsurance, and deductible amounts.
You may obtain further information about: 1) the status of providers by calling the toll-free telephone number on your identification card (or at myuhc.com); and
2) information on out-of-pocket expenses by calling the claims number listed on your identification card.
Premium
You will be given at least a 31-day notice of any change in your premium. We will make no change in your premium solely because of claims made by a covered person under the policy.
Reimbursement
If dental services are caused by the acts or omissions of a third party we have the right to be reimbursed to the extent of benefits we paid for dental services, as outlined in the policy.
Renewability
The policy term begins as of the effective date of the policy. You may keep the policy in force by paying us the required premium as it comes due. Your policy auto-renews as long as the premium is paid. However, we may cancel the policy if there is fraud or a material misrepresentation made by or with the knowledge of a covered person in filing a claim for benefits.
Termination
The policy will terminate:
• If you fail to pay the premiums when due, subject to the Grace Period defined in the policy;
• On the date you request;
• If we decline to renew all policies issued on this form with the same type and level of benefits in your state of residence; or
• On the date of your death, if your spouse is not covered under this plan.
Dependents
Eligible dependents are your lawful husband or wife and eligible children. Eligible children must be unmarried (and under 26 years of age at time of application.
Effective Date
For an application sent by electronic means, the effective date will be the later of: (i) the requested effective date; or (ii) the day after receipt by Golden Rule Insurance Company (GRIC). For a mailed application, the effective date will be the later of: (i) the requested effective date; or (ii) the day after the postmark date affixed by the U.S. Postal Service. If mailed and not postmarked by the U.S. Postal Service or if the postmark is not legible, the effective date will be the later of: (i) the requested effective date; or (ii) the date received by GRIC.
Health Insurance for Dental Expenses
If a covered person has other dental or health insurance that pays for expenses covered by the policy, we will not make payment until we determine what benefits are first paid by the other policy. Our payment will be reduced by the amount paid by the other plans.
Non-Network vs. Network Providers
Warning: You will pay more using non-network providers for non-emergency services. Non-network providers may bill you for any amount up to the billed charge after the plan has paid its portion. The basis of your benefit payment will be determined according to your policy’s non-network provider reimbursement.
No benefits are payable for:
- Any dental service relating to teeth that can be restored by other means; for purposes of periodontal splinting; to correct abrasion, erosion, attrition, bruxism, abfraction, or for desensitization; or teeth that are not periodontally sound or have a questionable prognosis.
- Orthodontia, braces, cosmetic dentistry, or dental implants.
- Oral surgery, except as expressly provided for in the policy.
- Orthognathic surgery, changing vertical dimension, restoring occlusion, bite analysis, or congenital malformation.
- Setting of facial bony fractures and any treatment associated with the dislocation of facial skeletal hard tissue.
- Treatment of malignant or benign neoplasms, cysts, or other pathology, except excisional removal.
- Mouthguards, precision or semi-precision attachments, occlusal guard, replacement of orthodontic retainers, treatment splints, bruxism appliance, duplicate dentures, harmful habit appliances, replacement of lost or stolen appliances, sleep disorder appliance, and gold foil restorations (except as provided for in the policy). For Major Services, no benefits are payable for:
- Initial placement of full or partial dentures or bridges and related services, to replace functional natural teeth that are: – Congenitally missing; or- Lost before insurance under the policy is in effect.
- Replacement of full or partial removable dentures, bridges, crowns, inlays, onlays, or veneers which can be repaired or restored to natural function.
• Replacement within 60 consecutive months of the last placement for full and partial dentures, and replacement within 60 consecutive months of the last placement for crowns, bridges, inlays, onlays, and veneers. This exclusion does not apply if the replacement is necessary because of extraction of a functioning natural tooth; or a present crown, bridge, or denture is temporary and a permanent crown, bridge, or denture is installed within 12 months from the date the temporary service was installed.
• Replacement of crowns, bridges, dentures, and fixed or removable prosthetic appliances inserted prior to plan coverage unless the covered person has been insured under the plan for 12 continuous months. If loss of a tooth requires the addition of a clasp, pontic, and/or abutment(s) within this 12-month period, dental services associated with the addition will be covered when the service is a covered expense.
• Replacement of complete dentures, fixed and removable partial dentures or crowns if damage or breakage was directly related to provider error. This type of replacement is the responsibility of the dentist. If replacement is necessary because of your or your dependents’ non-compliance, you are liable for the cost of the replacement.
• Fixed or removable prosthodontic restoration procedures for complete oral rehabilitation or reconstruction.